When you hear the phrase remineralizing gum, it sounds like marketing.
Teeth don’t regrow. Enamel doesn’t heal the way skin does. And chewing gum will never replace brushing, flossing, or professional dental care.
That skepticism is warranted.
But it’s also incomplete, because remineralizing doesn’t mean regrowing enamel. It means supporting a process your mouth naturally performs: re-hardening enamel that has been softened by acid before it becomes permanent damage and results in a mouth full of cavities.
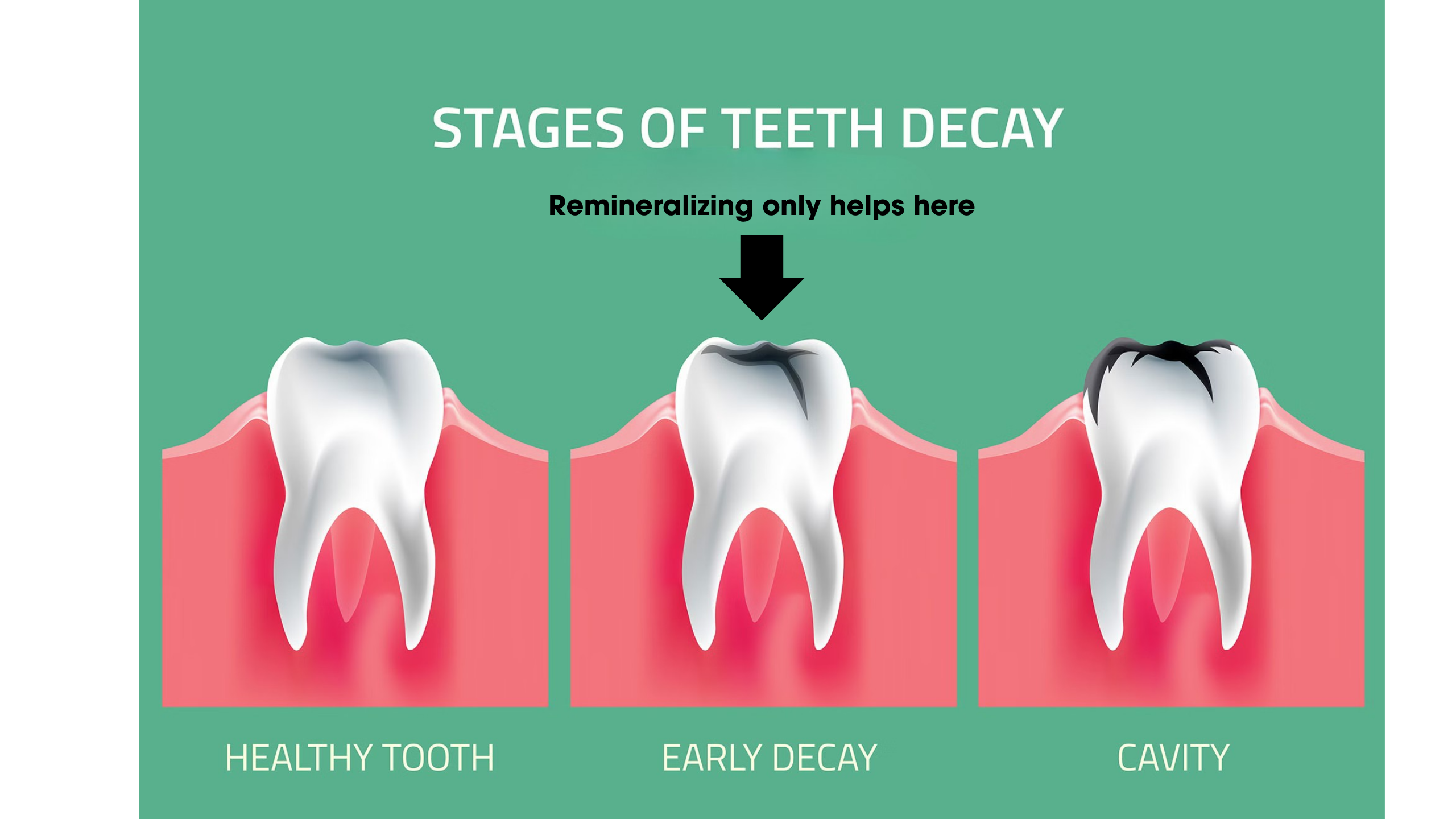
This is not a trivial distinction, because understanding that difference sets the proper expectations for what remineralizing gum is and is not capable of doing.
To set expectations most effectively, let’s start by looking at how regular gum affects oral hygiene and dental health.
How chewing regular gum already helps remineralization
Clinical research shows that chewing gum—when used deliberately after meals—can support this natural repair process beyond what brushing with fluoride toothpaste alone achieves.
Now this isn’t because gum contains a miracle ingredient, but rather, because chewing stimulates saliva, and saliva is the primary driver of acid neutralization and mineral recovery in the mouth.
So the question isn’t whether gum can replace oral hygiene. It can’t.
The real question is whether chewing gum at the right times can meaningfully reduce acid exposure and help stabilize early enamel damage before it becomes irreversible.
To answer that, we need to look at what the research actually tested—and what it found.
A 1992 Journal of Dental Research study had participants wear “dental appliances containing early-stage artificial enamel lesions.” Now there’s a lot I need to unpack in that sentence so that we’re on the same page.
- Dental appliances. Think of these as mouthguards coated with real tooth enamel. The participants in the study wore the dental appliances continuously, including during meals and sleep, for 7 weeks.
- Early-stage artificial enamel lesions. An enamel lesion is an early, reversible stage of tooth damage. A cavity occurs when an enamel lesion becomes irreversible. At that point, you need a filling.
Everyone brushed twice daily with a standard fluoride toothpaste. The only difference was that during the test phase, subjects also chewed gum five times per day for 20 minutes after meals and snacks.
Two types of gum were tested:
- Sugar-free gum (sorbitol-based)
- Sugar-containing gum
The goal was to see whether chewing itself could enhance enamel repair.
Across both gum types, chewing gum after meals led to greater remineralization of early enamel lesions compared to brushing alone. The effect was modest, but consistent enough to matter (Creanor et al., 1992).
The key mechanism wasn’t a special ingredient or coating. It was saliva.
Chewing gum dramatically increases saliva flow. Saliva:
- Neutralizes acid after eating
- Raises plaque pH
- Supplies calcium and phosphate ions needed for enamel repair
In short, chewing gum creates a more favorable environment for enamel to repair itself.
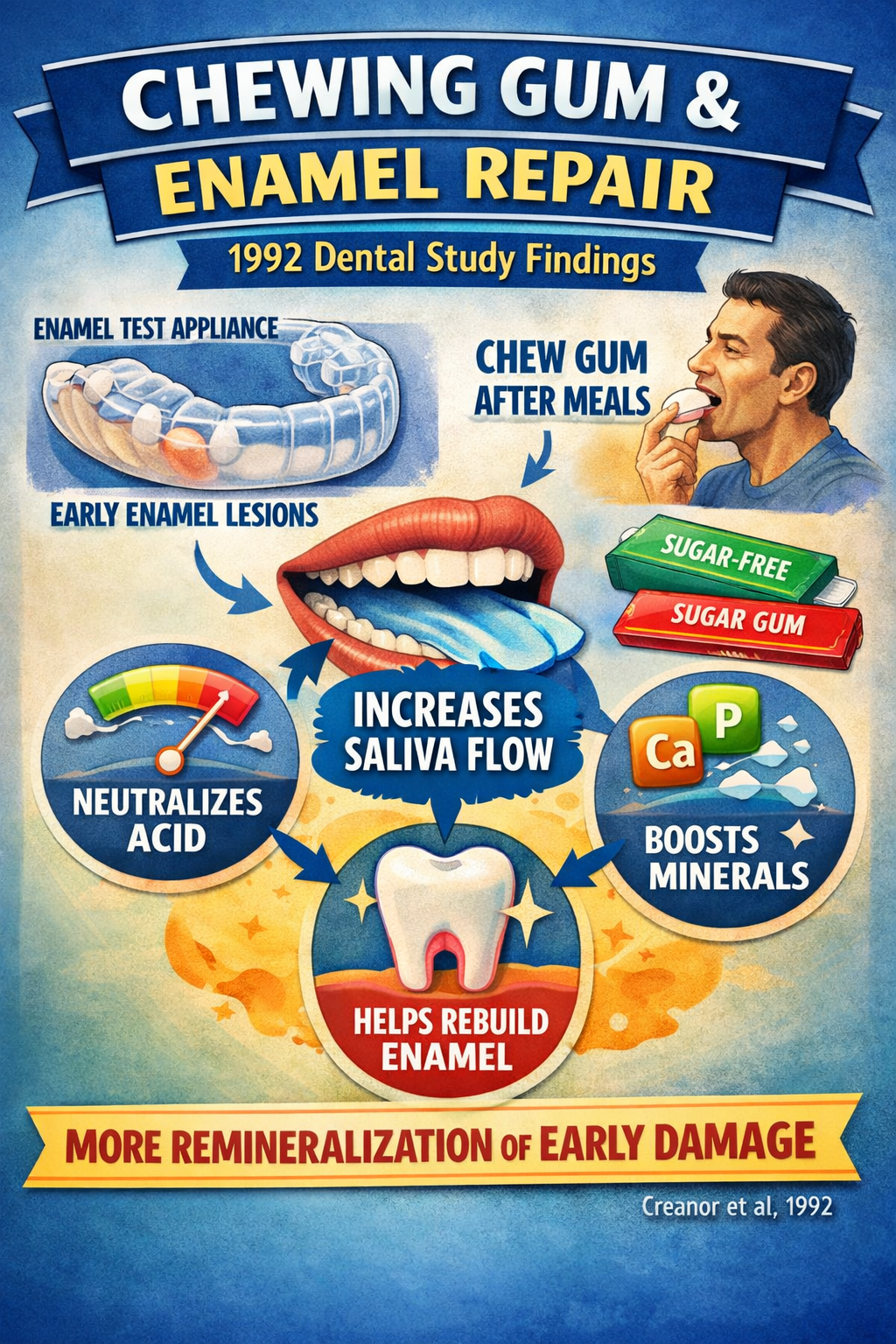
Interestingly, even sucrose-containing gum did not harm remineralization when chewed after meals for the full 20-minute period. Sugar is destructive to the teeth, but the increased saliva flow neutralized acids quickly enough that mineral recovery still occurred.
Based on the outcomes of the research, any chewing gum can accomplish this, whether it’s marketed as remineralizing gum, mastic gum, or if it’s just old fashion bazooka joe candy loaded with sugar.
So, the question naturally begs,”Is there anything special about remineralizing gum, and if so, which brands of remineralizing gum are better to use?”
To answer that question, we must examine the ingredient profiles of major brands of remineralizing gum—The VanMan Shop, Larine Co. and Nathan & Sons—and the science behind each ingredient.
 Xylitol: It tastes sweet, but it’s not sugar (The VanMan Shop., Larine Co., Nathan & Sons)
Xylitol: It tastes sweet, but it’s not sugar (The VanMan Shop., Larine Co., Nathan & Sons)
Xylitol is a naturally occurring sugar alcohol found in small amounts in fruits and vegetables. Chemically, it resembles sugar, and to your taste buds, it behaves like sugar. But to oral bacteria, it functions very differently.
Under normal conditions, enamel damage follows a predictable pattern. After eating sugar or refined carbohydrates, oral bacteria metabolize those sugars and produce acid.
That acid lowers plaque pH and pulls minerals—primarily calcium and phosphate—out of enamel. Remineralization—the process of allowing calcium and phosphate to rebuild in your teeth—can occur only after the acidic environment is neutralized.
Xylitol helps interrupt this cycle because oral bacteria, particularly Streptococcus mutans, cannot efficiently metabolize xylitol.
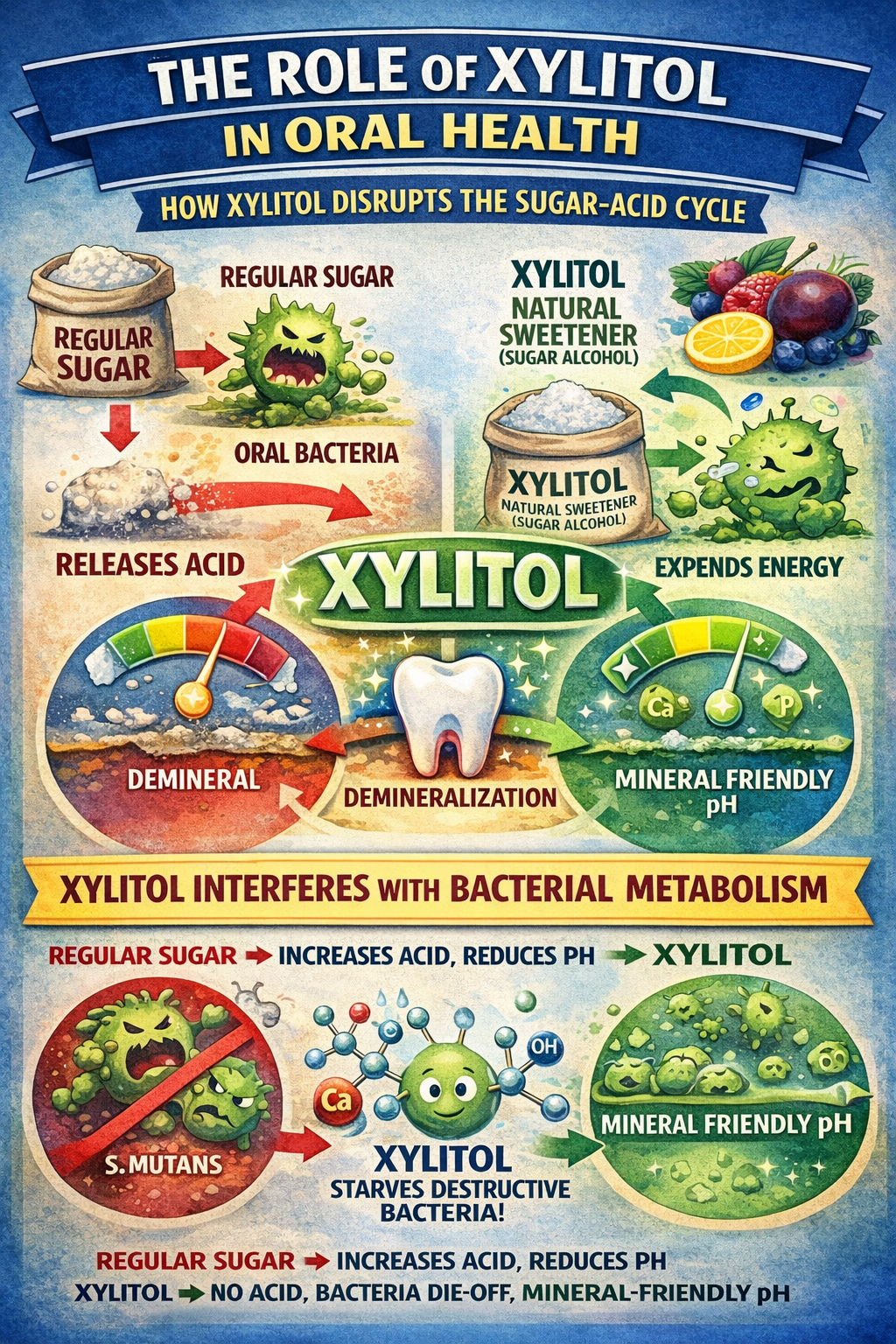
When bacteria try to break down xylitol for fuel, they expend energy without producing acid. This inefficient conversion reduces both acid production and the number of bacteria as they can not survive without fuel.
Chewing xylitol-containing gum also stimulates saliva flow, which helps buffer acids and restore a mineral-friendly pH.
Clinical research supports this mechanism. In controlled studies examining xylitol-sweetened chewing gum, regular use has been associated with enhanced remineralization of early enamel subsurface lesions, compared to no gum use, under conditions that promote saliva stimulation and pH recovery (Mäkinen et al., 2009).
It’s important to be precise about what this means.
Xylitol does not rebuild enamel or repair cavities. Instead, it reduces ongoing demineralization and helps create oral conditions in which saliva can naturally re-harden weakened but not structurally damaged enamel. Xylitol accomplishes this by starving the destructive bacteria of their food source.
Why does every remineralizing gum use xylitol?
Xylitol meets several requirements that no other sweetener satisfies as reliably. Xylitol:
- Provides sweetness without feeding acid-producing bacteria
- Supports neutral plaque pH
- Stimulates saliva through chewing
- Has a substantial body of dental research behind it
A note on “organic xylitol.”
The VanMan Company states that it uses organic xylitol, which deserves clarification.
Strictly speaking, xylitol itself cannot be USDA-certified organic in the traditional sense. It is a purified compound that must be extracted and purified from plant material, a process that typically precludes formal organic certification.
What the VanMan Company—and other companies that use the designation organic xylitol—typically mean is that the xylitol is plant-derived, sourced from non-GMO materials, and produced under cleaner processing standards.
In this context, “organic” functions more as a sourcing and quality signal than as a regulated certification claim.
Erythritol: Sweetness without acid (Nathan & Sons, Larine Co.)
If xylitol is the “anti-acid” sweetener, erythritol is the “don’t-feed-plaque + easier-on-the-gut” sweetener that helps people actually stick with the habit.
Erythritol, like xylitol, is a naturally occurring sugar alcohol found in small amounts in fruits and fermented foods. It fits the same profile as xylitol, in that it tastes sweet but does not behave like sugar in the mouth. However, its role in remineralizing gum is slightly different.
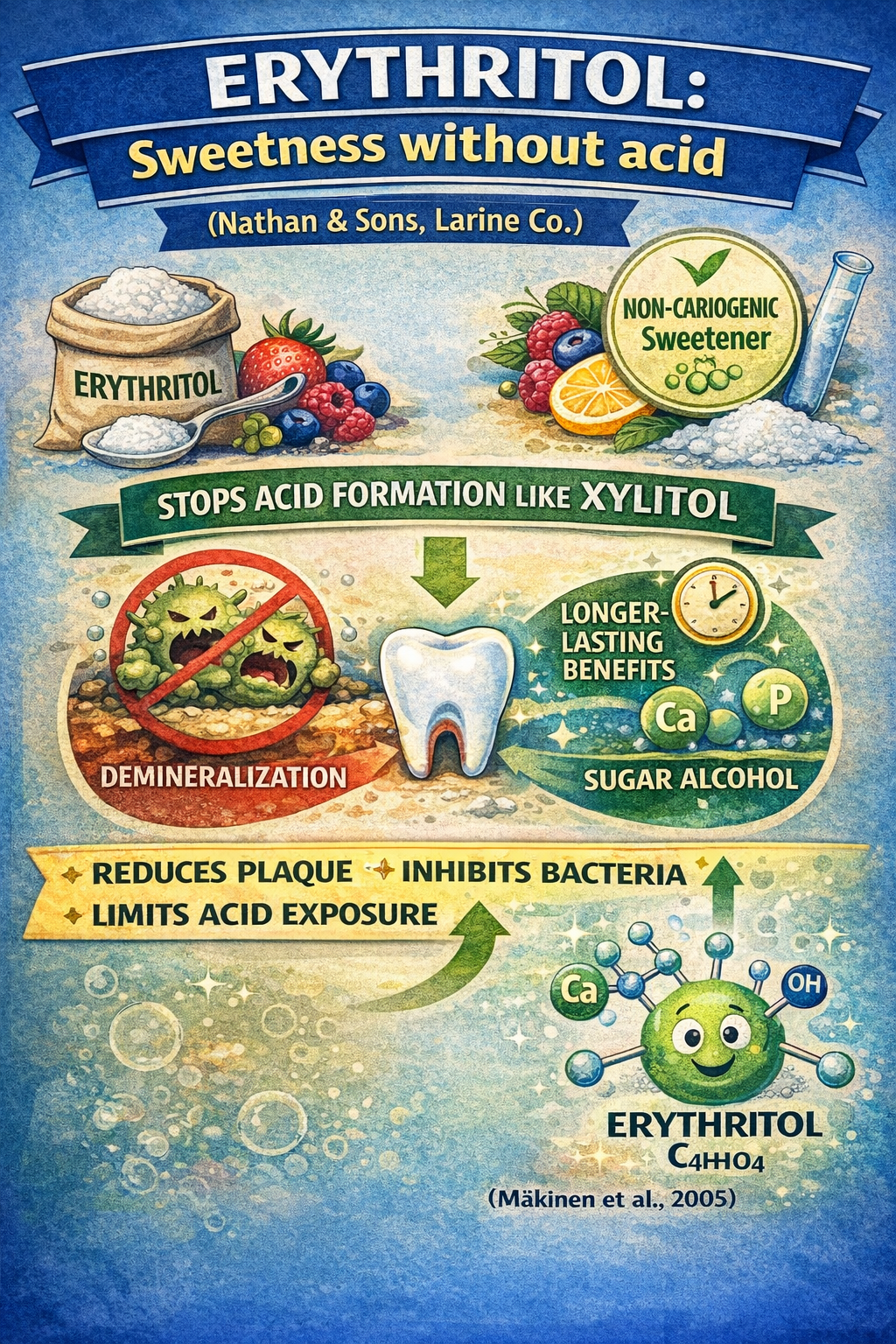
From an oral-health perspective, erythritol is best understood as a non-cariogenic supporting sweetener rather than a direct remineralizing agent.
As with xylitol, oral bacteria cannot ferment erythritol to produce acid, which means it stops bacteria through the same starvation method. Additionally, research suggests erythritol may interfere with bacterial growth and plaque formation by reducing bacterial adhesion to tooth surfaces, further limiting acid exposure over time (Mäkinen et al., 2005).
Why do some remineralizing gums use erythritol alongside xylitol?
Nathan & Sons and Larine Co. include erythritol in addition to xylitol for practical and functional reasons.
Erythritol allows brands to maintain sweetness without feeding acid-producing bacteria. The added sweetness of both sugars encourages longer and more consistent chewing. Longer chewing increases saliva flow, and that’s where all the remineralization magic happens.
Erythritol is functionally similar to xylitol, but using them together can improve real-world usability and consistency, which ultimately matters more than theoretical maximum dosing.
Hydroxyapatite (The VanMan Shop., Larine Co., Nathan & Sons)
Hydroxyapatite is the primary mineral that makes up tooth enamel and dentin. In fact, roughly 95–97% of enamel by weight is composed of hydroxyapatite crystals arranged in a highly organized structure.

That single fact explains why hydroxyapatite shows up in nearly every serious remineralizing gum formulation.
While all three companies use hydroxyapatite, the type each uses differs slightly. It’s included in all three because hydroxyapatite is one of the few ingredients that can plausibly contribute to true remineralization of early enamel damage, rather than merely reducing further harm (Amaechi et al., 2019).
Nano-Hydroxyapatite vs. Hydroxyapatite (What the “Nano” Actually Changes)
Hydroxyapatite is hydroxyapatite. The “nano” or “micro” version isn’t a different mineral—it’s the same material, just manufactured in a much smaller particle size.
That sounds like a trivial distinction, but particle size changes how the ingredient behaves in the mouth, and it’s the main reason brands highlight the size on the label.
Regular hydroxyapatite is typically made of larger particles. In practice, that means it tends to work more like a surface-level filler: it can settle onto softened enamel, help smooth microscopic roughness, and contribute to re-hardening where the enamel is still intact.
Nano-hydroxyapatite is the same mineral, but the particles are closer to the scale of natural enamel crystals. Because they’re smaller, they can fit into smaller pores and defects in early enamel lesions more easily, at least in theory. That’s why nano-hydroxyapatite is often positioned as “more biomimetic” or “closer to real enamel.”

However, “nano,” or “micro” distinction doesn’t change what remineralization can do. It just changes how efficiently the mineral may deliver in early-stage damage.
Hydroxyapatite, regardless of the size or type, still does not regrow enamel or repair cavities.
It can only help when the enamel is still intact, the lesion is early and reversible, pH level enables mineral recovery, and saliva is present to transport and buffer
And that last point is key in a gum context.
In toothpaste, nano-hydroxyapatite gets actively brushed into the enamel surface and sits there longer. In gum, the mineral is delivered through saliva while you chew, and the dominant factor remains the same: saliva flow and pH recovery.
So, is nano-hydroxyapatite “better”? Potentially—but the advantage is likely too small to notice.
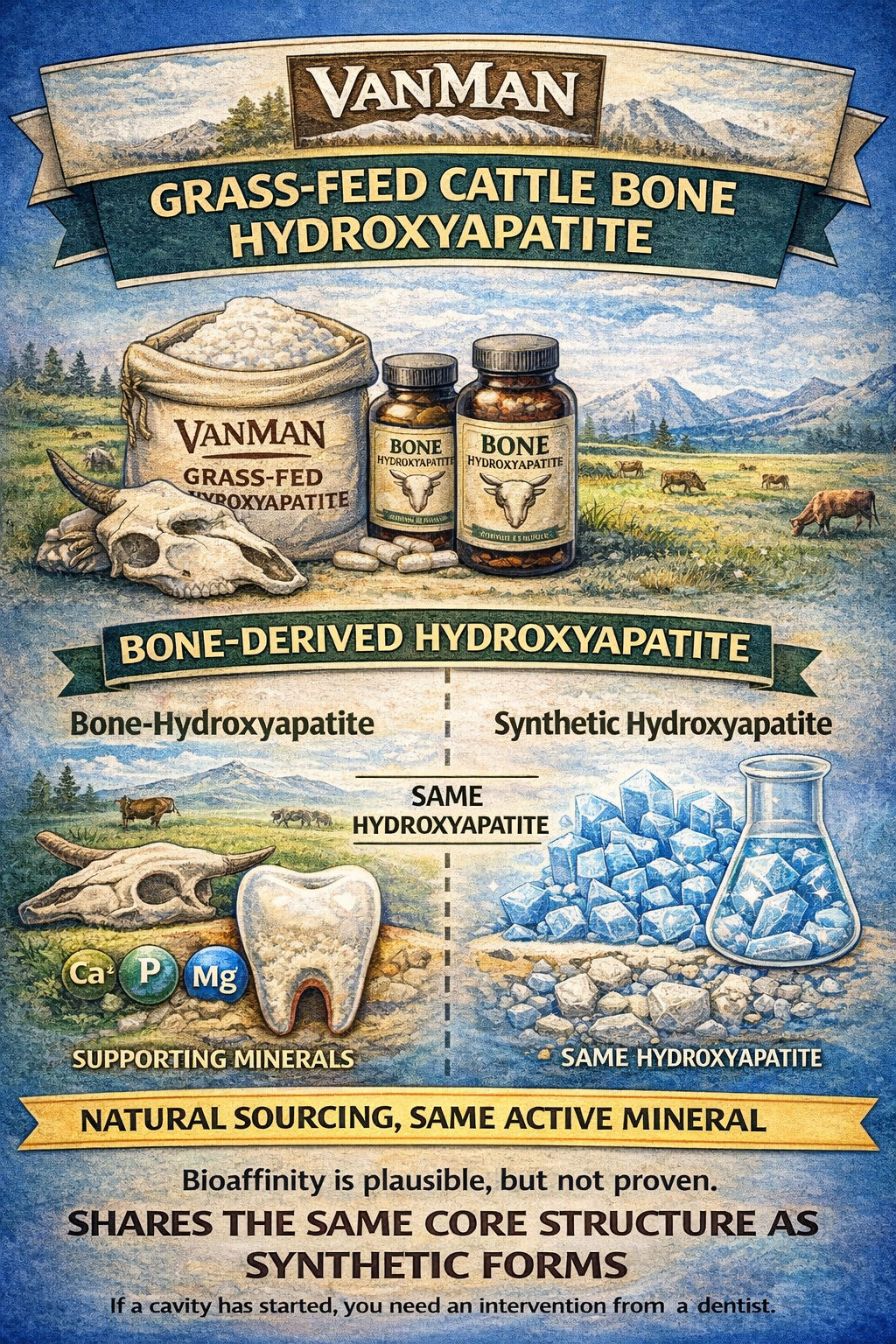
VanMan’s use of grass-fed cattle bone hydroxyapatite
While Nathan & Sons and Larine Co. use synthetic hydroxyapatite, The VanMan Company specifies that it uses grass-fed cattle bone hydroxyapatite.
From a chemical standpoint, bone-derived hydroxyapatite and high-quality synthetic hydroxyapatite share the same core structure. In both cases, the active component interacting with enamel is hydroxyapatite itself.
There is no strong clinical evidence showing that bone-derived hydroxyapatite remineralizes enamel more effectively than synthetic forms when particle size and formulation are comparable.
Where the difference may matter is in sourcing and composition. Bone-derived hydroxyapatite naturally contains small amounts of calcium, phosphorus, magnesium, and other trace minerals present in human teeth.
In theory, this closer resemblance to biological mineral matrices could support bioaffinity, but this remains plausible rather than proven in dental outcomes.
VanMan’s choice should be understood as a preference for natural sourcing and minimal processing, rather than as a guarantee of increased remineralization performance.
For some users, that distinction may matter. Bone-derived hydroxyapatite may appeal to those who prefer naturally derived minerals rather than synthetics, but it doesn’t make them any more or less effective.
The special gum in remineralizing gum
In addition to sweeteners like xylitol and erythritol, remineralizing gums rely on a base made from natural plant resins.
These ingredients don’t remineralize enamel directly, but they play an important supporting role by enabling chewing, influencing saliva flow, and shaping the oral environment.
This is the first ingredient class in which brands make markedly different choices.
Understanding what each of these gums does helps clarify why they’re used—and why some brands choose fewer of them.
Chicle gum: The saliva-producing foundation (The VanMan Shop, Larine Co., Nathan & Sons)
Chicle gum is a natural latex harvested from the sapodilla tree and was the original base used in chewing gum before synthetic rubbers became common.
Little known fun fact:
Chiclets gum is named after chicle gum and was invented by an exiled Mexican president. True story.
Its primary role in remineralizing gum is structural.
Chicle provides firm, elastic chew resistance that breaks down slowly over time. This allows for longer, more consistent chewing sessions without the gum dissolving or turning sticky too quickly.
That matters because saliva stimulation is the dominant driver of remineralization.
The longer and more steadily someone chews, the more saliva is produced, and the more effectively acids are buffered, and minerals are carried back to weakened enamel.
Mastic gum: Bacterial pressure control (The VanMan Shop., Larine Co., Nathan & Sons)
Mastic gum is a resin from the mastic tree (Pistacia lentiscus), traditionally chewed in Mediterranean regions for oral and digestive health.
Further reading: The Best Mastic Gum—A Comprehensive Review
In the context of remineralizing the oral environment, mastic gum primarily serves as an oral environmental support. It exhibits mild antimicrobial activity that may reduce bacterial load in the oral cavity, particularly bacteria implicated in plaque formation and acid production (Karygianni et al., Front Microbiol, 2016).
Mastic gum also contributes to chewing resistance, though less so than chicle. When paired together, chicle provides durability, while mastic gum helps keep bacteria in your mouth under control.
Myrrh gum: Inflammation and microbial balance (Larine Co., Nathan & Sons)
Myrrh gum is a resin from the Commiphora species and has a long history of use in oral hygiene products and preparations.
Its primary contribution in remineralizing gum is antimicrobial and anti-inflammatory support. Myrrh has been shown to inhibit certain oral bacteria and may help soothe the gums and reduce low-grade oral inflammation (Anwar et al., 2025).
 While this does not directly affect enamel mineral content, gum health and inflammation influence the overall oral environment. Chronic inflammation and bacterial imbalance can increase acid exposure and interfere with saliva’s protective role.
While this does not directly affect enamel mineral content, gum health and inflammation influence the overall oral environment. Chronic inflammation and bacterial imbalance can increase acid exposure and interfere with saliva’s protective role.
Myrrh gum appears to function as a supportive adjunct, creating an environment that facilitates remineralization while generally improving oral health.
Acacia gum: Texture, binding, and stability (Larine Co., Nathan & Sons)
 Acacia gum, also known as gum arabic, is derived from the sap of acacia trees and is widely used in food and pharmaceutical applications.
Acacia gum, also known as gum arabic, is derived from the sap of acacia trees and is widely used in food and pharmaceutical applications.
This gum doesn’t provide any antibacterial or antimicrobial benefits. Rather, it adds more support and texture to remineralizing gum. It acts as a binder and stabilizer, helping ingredients hold together.
There is limited evidence suggesting that acacia gum may have mild protective or prebiotic effects in the mouth, but it’s primarily used as a structural gum base. In fact, it’s a fairly common emulsifier and thickener in foods, beverages, and cosmetics.
Why does VanMan Shop only uses chicle and mastic?
The VanMan Company’s decision to use only chicle and mastic gum appears to reflect a strategy of choosing the “minimally effective dose.”
Chicle alone provides chewing resistance and saliva stimulation. I did not observe any consistency issues when chewing VamMan Remineralizing Gum.
While I haven’t personally tried Nathan & Sons or Larine Co., I can’t imagine the chewing experience is substantially better because of the inclusion of acacia gum.
However, I have chewed mastic gum on several occasions, and let me tell you, it’s tough. Mastic is famously tough (people even chew it for jaw training), so from a pure ‘keep chewing longer’ standpoint, it does the job.
In other words, if the chicle gum didn’t add to chewing consistency, the mastic gum certainly does.
The Vanman Company also does not use myrrh gum. I don’t really understand what Nathan & Sons and Larine Co. use it for, considering that mastic gum has been studied specifically in the context of chewing, saliva stimulation, and plaque-related bacteria, whereas myrrh is more commonly studied as an extract or topical agent.
Moreover, once bacterial acid production is suppressed, adding additional antimicrobial agents typically yields diminishing returns for enamel remineralization.
The one thing myrrh gum does that mastic gum does not is have noted anti-inflammatory properties.
This can certainly assist in remineralization if the cause is periodontal disease (e.g., gingivitis), but oral inflammation is not typically a cause or effect of the dental lesions that develop into cavities.
Why The VanMan Shop limits its remineralizing gum formula to just six ingredients
After breaking down each component individually, the more interesting question is why VanMan stops where it does.
The VanMan Company’s remineralizing gum contains only six ingredients:
- Chicle gum
- Mastic gum
- Organic xylitol
- Grass-fed cattle bone hydroxyapatite
- Organic peppermint extract
- Organic peppermint oil
That’s an unusually short list for a product operating in a category where it’s easy to stack additives, resins, sweeteners, and flavor systems. The decision appears intentional, not incidental.
A focus on primary mechanisms, not redundancy
VanMan’s ingredient list hits the core mechanisms of remineralizing gum without any extras or overlap.
- Chicle gum provides structural chew resistance and durability
- Mastic gum adds additional resistance and antimicrobial pressure
- Xylitol reduces acid production and supports pH stability
- Grass-Feed Cattle Bone Hydroxyapatite supplies an enamel-compatible mineral material
- Peppermint extract and oil support flavor, saliva stimulation, and mild antimicrobial activity (Karygianni et al., 2016)
This suggests a formulation philosophy aimed at covering each necessary function once, rather than stacking multiple ingredients with overlapping roles.
Preference for whole, functional ingredients over engineered blends
Another consistent pattern is VanMan’s preference for whole or minimally processed ingredients over engineered systems.
Instead of:
- Synthetic gum bases
- Synthetic hydroxyapatite
- Isolated terpene blends
- Multi-sweetener flavor systems
VanMan relies on:
- Chicle and mastic gum for chew mechanics
- Peppermint extract and oil for flavor and sensory stimulation
This approach makes the formulation easier for consumers to understand and evaluate—an important consideration in a category where marketing claims often exceed reality.
The cost and pricing structure of remineralizing gum
Looking at the ingredient lists alone tells you part of the story. Looking at how each company prices and sells its gum fills in the rest.
Here’s how the three major brands structure their pricing:
- The VanMan Company. $12 for a one-time purchase or $10 with a monthly subscription
21 pieces per pack - Nathan & Sons. Sold only in two-pack bundles. $29.99 one-time or $20 with a monthly subscription. 36 pieces total
- Larine Co. $20 for two packs. 36 pieces total. No subscription option
At first glance, these prices seem broadly similar. But when you break them down, the differences point to very different assumptions about how the gum will be used.
VanMan Shop: low commitment, frequent use
VanMan’s pricing is structured around accessibility and experimentation.
By offering a single pack at a relatively low price, the product appears designed for people who want to try remineralizing gum without committing to bulk purchases or recurring shipments.
The per-piece cost is higher, but the upfront commitment is lower. That suggests VanMan expects users to evaluate the gum as a supplemental habit—something you add to an existing oral-care routine, not something you stockpile.
The subscription discount incentivizes consistency without forcing it,
Nathan & Sons: subscription-first, habit replacement
Nathan & Sons takes a very different approach.
By selling only in two-pack bundles and heavily discounting subscriptions, the pricing structure incentivizes customers to adopt regular, ongoing use at scale. This suggests an expectation that users will chew the gum daily, multiple times per day, and view it as a core oral-care habit rather than an occasional support tool.
The lower per-piece cost makes sense in that context. The product is positioned less like a specialty gum and more like a daily-use consumable, in which volume and repeat purchases matter.
Larine Co.: transactional, no habit lock-in
Larine Co.’s pricing sits somewhere in between, but its lack of a subscription option is telling.
By offering a two-pack at a flat price with no recurring model, Larine appears to treat remineralizing gum as a one-off or periodic purchase, rather than a habit-forming product. This suggests positioning closer to a specialty oral-care product than to a daily-use staple.
Taken together, the pricing structures suggest three distinct philosophies:
- VanMan emphasizes low entry cost, optional consistency, and minimalist use
- Nathan & Sons emphasizes routine, volume, and subscription-driven behavior
- Larine Co. emphasizes straightforward value without ongoing commitment
None of these approaches is inherently better. They simply reflect different assumptions about how remineralizing gum fits into a person’s life.
A product that encourages moderate, sustainable use may outperform one designed for aggressive daily chewing if the latter leads to fatigue or drop-off.
VanMan prices its gum like a targeted supplement.
Nathan & Sons prices its gum like a daily staple.
Larine Co. prices its gum like a specialty product.
Understanding those assumptions clarifies who each product is actually designed for—and why the formulations look the way they do.
Remineralizing gum comparison: Ingredients, philosophy, and use case
If you want the quick answer first, here’s how the three brands compare.
The basic philosophy of each brand of remineralizing gum:
- VanMan → minimalist, targeted, supplement-style
- Nathan & Sons → comprehensive, daily-use, subscription-driven
- Larine Co. → natural-mineral approach without habit lock-in
- Regular gum → taste and freshness, no enamel support
What remineralizing gum is good for (And who it’s for)
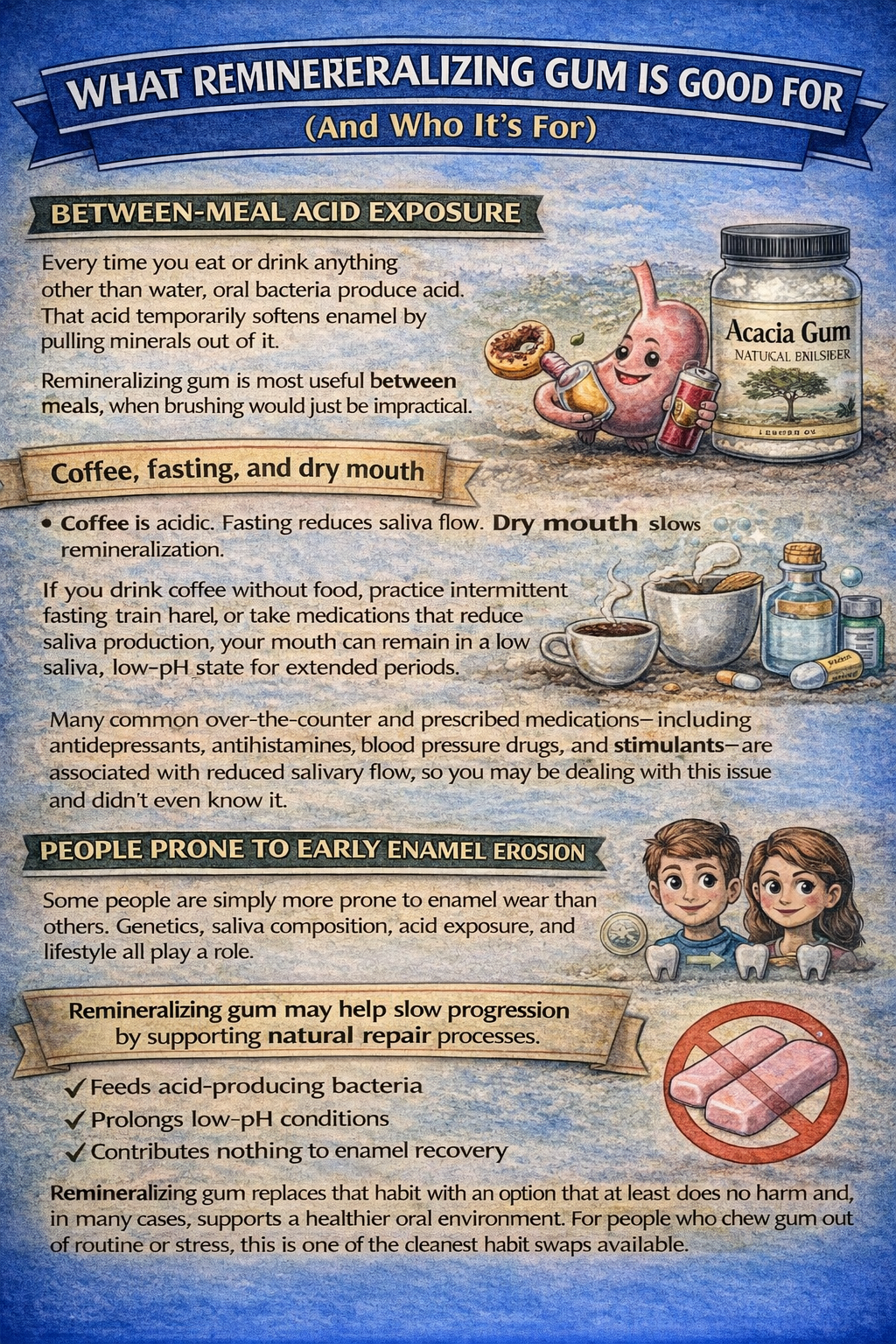
Between-meal acid exposure
Every time you eat or drink anything other than water, oral bacteria produce acid. That acid temporarily softens enamel by pulling minerals out of it.
Remineralizing gum is most useful between meals, when brushing would just be impractical.
This is particularly relevant if you snack frequently or consume beverages throughout the day.
Coffee, fasting, and dry mouth
Coffee is acidic. Fasting reduces saliva flow. Dry mouth slows remineralization.
If you drink coffee without food, practice intermittent fasting, train hard, or take medications that reduce saliva production, your mouth can remain in a low-saliva, low-pH state for extended periods.
Many common over-the-counter and prescribed medications—including antidepressants, antihistamines, blood pressure drugs, and stimulants—are associated with reduced salivary flow, so you may be dealing with this issue and didn’t even know it.
People prone to early enamel erosion
Some people are simply more prone to enamel wear than others. Genetics, saliva composition, acid exposure, and lifestyle all play a role.
Although no single gene determines enamel erosion risk, research indicates that genetic factors influencing enamel quality and salivary protection contribute to individual differences in susceptibility to erosion under acid exposure.
Twin and genetic studies indicate that these traits are partially heritable, meaning that a subset of the population has a higher baseline vulnerability, whereas clinical outcomes remain strongly shaped by environmental factors such as diet, saliva, and oral habits (Vieira, 2014; Haworth et al., 2020).
Remineralizing the gum may help slow progression by supporting natural repair processes, provided the enamel remains intact.
People quitting sugar gum
Switching from conventional sugar or artificially sweetened gum to remineralizing gum can be a meaningful upgrade.
Traditional gum may freshen breath, but it often:
- Feeds acid-producing bacteria
- Prolongs low-pH conditions
- Contributes nothing to enamel recovery
Remineralizing gum replaces that habit with an option that at least does no harm and, in many cases, supports a healthier oral environment.
For people who chew gum out of routine or stress, this is one of the cleanest habit swaps available.
What remineralizing gum is not good for
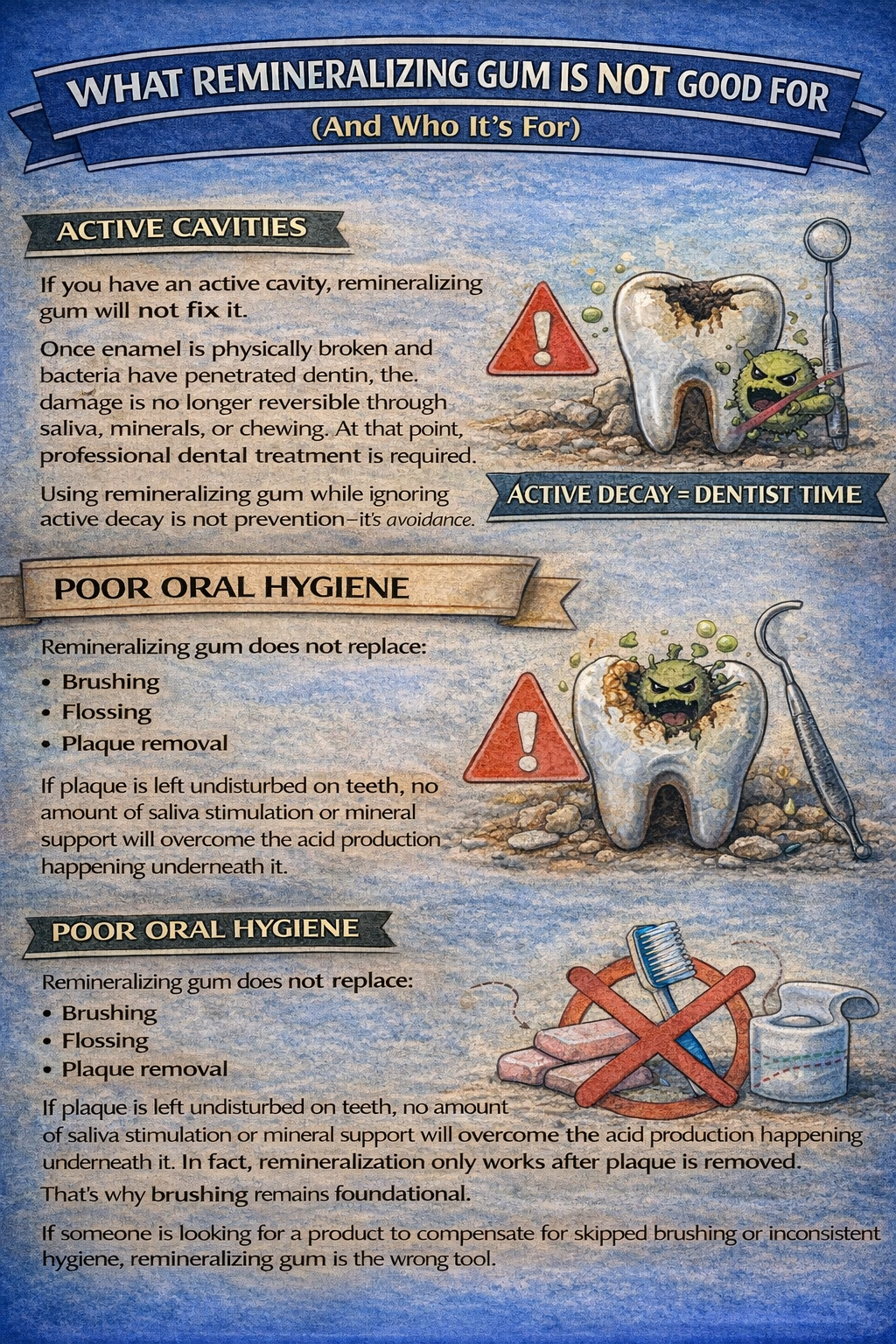
Active cavities
If you have an active cavity, remineralizing gum will not fix it.
Once enamel is physically broken and bacteria have penetrated dentin, the damage is no longer reversible through saliva, minerals, or chewing. At that point, professional dental treatment is required.
Using remineralizing gum while ignoring active decay is not prevention—it’s avoidance.
Poor oral hygiene
Remineralizing gum does not replace:
- Brushing
- Flossing
- Plaque removal
If plaque is left undisturbed on teeth, no amount of saliva stimulation or mineral support will overcome the acid production happening underneath it.
In fact, remineralization only works after plaque is removed. That’s why brushing remains foundational.
If someone is looking for a product to compensate for skipped brushing or inconsistent hygiene, remineralizing gum is the wrong tool.
The right way to think about remineralizing gum
Remineralizing gum works best when you already have:
- Reasonable oral hygiene
- Intact enamel
- A desire to reduce small, repeated acid stress
It is a supportive tool, not a corrective one.
Used correctly, it helps tip the balance slightly back in your favor—especially in modern environments where constant eating, drinking, and dry mouth work against enamel.
Used incorrectly, it creates false confidence.
That distinction matters—not only for dental health, but also for selecting the appropriate product and having realistic expectations.
The best remineralizing gum to use is VanMan’s remineralizing gum

I’m a big fan of the minimalistic approach. Now I fully admit that I haven’t tried the others, but the taste and consistency are fine, and the price is lower than that of the other gums by almost 50% in some cases.
Feel free to try them, as they all have the same working basic ingredients—and the additional ingredients do no harm—but my personal stance is that they’re solid products.
VanMan’s just figured out a way to offer it at a price point and quality level that blows away the competition. 13k reviews can’t be wrong.
But if you don’t trust me, feel free to check out of the other brands. If you purchase at the links below, Ip receive a small commission at no extra cost to you.
Think of it as a way of saying “thank you” for helping you make an informed decision.
- Purchase VanMan’s Remineralizing Gum—my recommended choice—here.
- Purchase Nathan & Sons Underbrush Gum here.
- Purchase Larine Co. Remineralizing Gum here.
References
Amaechi, B. T., AbdulAzees, P. A., Alshareif, D. O., Shehata, M. A., Lima, P. P. C. S., Abdollahi, A., & Kalkhorani, P. S.
Comparative efficacy of a hydroxyapatite toothpaste and a fluoride toothpaste for prevention and remineralization of dental caries in children. BDJ Open. 2019;5:18.
https://doi.org/10.1038/s41405-019-0026-8
Anwar, M. A., Sayed, G. A., Hal, D. M., Hafeez, M. S. A. E., Shatat, A. S., Salman, A., Eisa, N. M., Ramadan, A., El-Shiekh, R. A., Hatem, S., & Aly, S. H.
Herbal remedies for oral and dental health: A comprehensive review of their multifaceted mechanisms including antimicrobial, anti-inflammatory, and antioxidant pathways. Inflammopharmacology. 2025;33(3):1085–1160.
https://doi.org/10.1007/s10787-024-01631-8
PMID: 39907951 · PMCID: PMC11914039
Creanor, S. L., Strang, R., Gilmour, W. H., Foye, R. H., Brown, J., Geddes, D. A. M., & Hall, A. F.
The effect of chewing gum use on in situ enamel lesion remineralization. Journal of Dental Research. 1992;71(12):1895–1900.
https://doi.org/10.1177/00220345920710120801
Haworth, S., Esberg, A., Lif Holgerson, P., Kuja-Halkola, R., Timpson, N. J., Magnusson, P. K. E., Franks, P. W., & Johansson, I.
Heritability of caries scores, trajectories, and disease subtypes. Journal of Dental Research. 2020;99(3):264–270.
https://doi.org/10.1177/0022034519897910
PMID: 31905308 · PMCID: PMC7036480
Karygianni, L., Al-Ahmad, A., Argyropoulou, A., Hellwig, E., Anderson, A. C., & Skaltsounis, A. L.
Natural antimicrobials and oral microorganisms: A systematic review on herbal interventions for the eradication of multispecies oral biofilms. Frontiers in Microbiology. 2016;6:1529.
https://doi.org/10.3389/fmicb.2015.01529
PMID: 26834707 · PMCID: PMC4712263
Mäkinen, K. K.
Sugar alcohols, caries incidence, and remineralization of caries lesions: A literature review. Caries Research. 2009;43(2):83–92.
https://doi.org/10.1159/000209344
Mäkinen, K. K., Saag, M., Isotupa, K. P., Olak, J., Nõmmela, R., Söderling, E., & Pienihäkkinen, K.
Similarity of the effects of erythritol and xylitol on some risk factors of dental caries. Caries Research. 2005;39(3):207–215.
https://doi.org/10.1159/000084800
PMID: 15914983
Vieira, A. R., Modesto, A., & Marazita, M. L.
Caries: Review of human genetics research. Caries Research. 2014;48(5):491–506.
https://doi.org/10.1159/000358333
PMID: 24853115 · PMCID: PMC4167926




